Many people find it difficult to talk about death and dying.
When confronted with the question of whether a mentally capable, terminally ill adult with six months or less to live should have the legal option to obtain prescription medication to avoid needless suffering and die peacefully, their initial reaction may be a negative or skeptical one. But countless lawmakers, healthcare professionals, religious leaders, scholars and everyday Americans are changing their minds about where they stand on this issue.
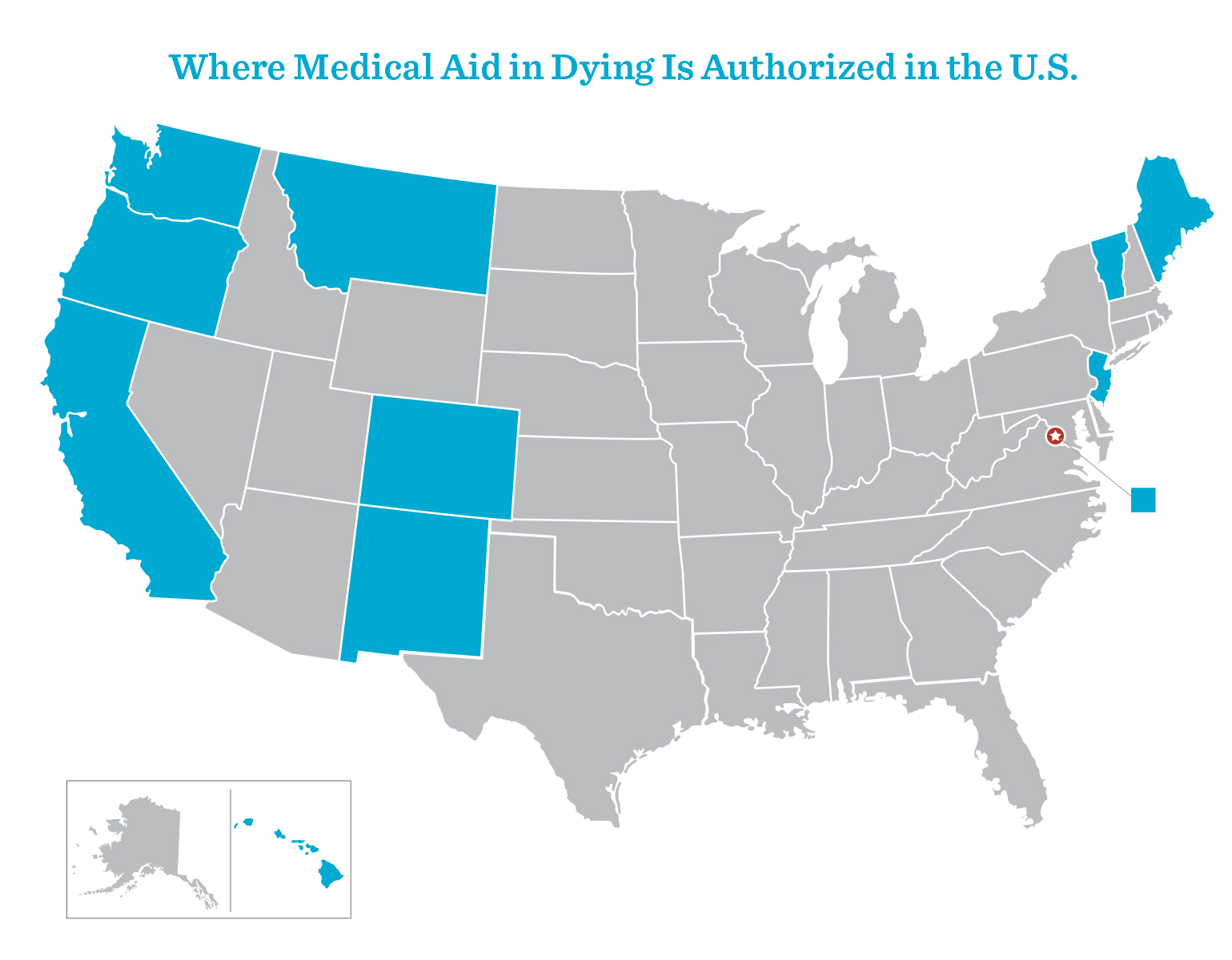
That’s because they are watching as the 11 U.S. jurisdictions (10 states and Washington, D.C.) that have authorized medical aid in dying and the evidence about how these laws are working show that the claims of abuse and coercion made by opponents of these laws never materialized. They are also hearing testimony from terminally ill advocates who urgently need the option of medical aid in dying and from advocates whose loved ones died suffering without the option.
People change their minds when this issue becomes personal for them: when they witness a loved one who dies in agony. As one convert, Connecticut State Senator Gary Winfield, observed, many people “are one bad death away from being a supporter.”
But perhaps most importantly, people with doubts about this option change their minds when they see the peace and comfort that just having this option brings terminally ill people and their families in Washington, D.C. and 10 states that allow it: California, Colorado, Hawai‘i, Maine, Montana, New Jersey, New Mexico, Oregon, Vermont and Washington State. The following pages include some voices reflecting the change of heart that many people have had about medical aid in dying.
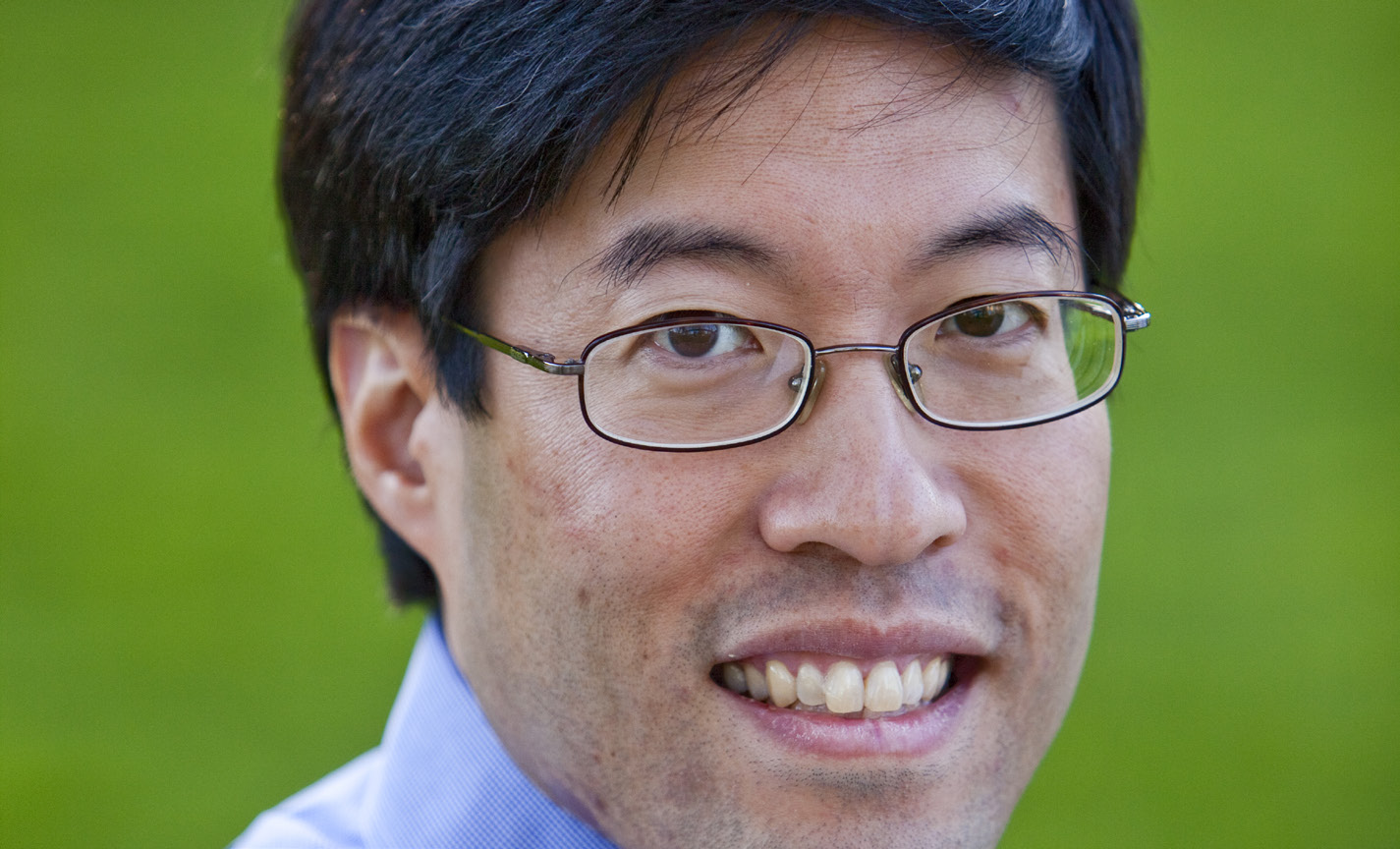
CALIFORNIA STATE SENATOR
Richard Pan, M.D.
Despite voting against the California End of Life Option Act in 2016, state Sen. Richard Pan, a physician who chaired the Senate Health Committee, voted to approve SB380, a 2021 amendment to improve access to medical aid in dying in California by shortening the waiting period from 15 days to 48 hours and streamlining the process of requesting aid-in-dying medication for patients and providers.
“I think it’s clear that this is something people in California want and we need to make sure [it] works, and that’s why I’m in support of this bill… there were a lot of protections in the original bill. I don’t think we’re weakening those protections at all with what you’re doing with this bill [shortening the waiting period from 15 days to 48 hours],” said Sen. Pan in a California Senate Health Committee Hearing in March 2021.
Source: California Senate Health Committee Hearing transcript, Mar. 24, 2021

CONNECTICUT STATE SENATOR
Saud Anwar, M.D.
Connecticut State Senator Saud Anwar, M.D., who chairs the Public Health Committee, used to be against medical aid-in-dying legislation, but after hearing numerous testimonies from people who are terminally ill, their families and friends as well as advocates, he changed his mind. He plans to bring Connecticut’s medical aid-in-dying bill (SB1076) up for a vote in 2024.
“If you look at the testimonies of the various legislators, they will tell you that they were a hard no at one point to the bill, myself included,” Sen. Anwar said. “But, over time, we realized the situation and how many people were impacted.”
Source: CT Examiner, “Advocates Work to Bring Medical Aid-in-Dying Bill Back in 2024,” Oct. 16, 2023

CONNECTICUT STATE SENATOR
Gary Winfield
For Connecticut State Sen. Gary Winfield, medical aid in dying was not an issue at the top of his mind as a lawmaker, but it became a painfully personal experience during the needlessly agonizing death of his mother. Winfield, co-chair of the Judiciary Committee, tearfully recalled at an April 19, 2023 committee meeting:
“This woman, who was a staple in our church, talked to me about what she believed at the end of her life. This person, who I never would have thought would think this, said to me one time that she wished she could die. And she meant on her own terms. There are a lot of us who are one bad death away from being a supporter.” Sen. Winfield has vocally advocated for the medical aid in dying option to become legal in Connecticut for almost a decade, and hopes to see a bill pass in 2024.
Sources: CT Mirror, “CT aid in dying bill won’t advance this year,” Apr. 19, 2023; New Haven Register, “State Sen. Gary Winfield: Aid in dying – the issue in Connecticut is choice,” Jan. 28, 2015

ILLINOIS PSYCHIATRIST
Dr. Cynthia Chatterjee
Illinois psychiatrist Dr. Cynthia Chatterjee was initially opposed to medical aid in dying, but as she learned more about the safeguards in place and looked at the abundant research available from other states, she became supportive of this end-of-life care option. That support grew when her father, a 94-year-old resident of Washington State where medical aid in dying is authorized, decided to utilize the option to peacefully end his suffering caused by a cardiac condition.
“Although I had no objection to my father’s opting for medical aid in dying, I had a lot of anxiety about the process. But once I observed his death, I was convinced that it was a compassionate act. After taking the medication, he fell asleep within three minutes, and died peacefully within 15 minutes. There was no struggling or gasping for breath, which had been his greatest fear. I came away from my father’s death wishing that everyone could have the opportunity to have such a peaceful passing,” Dr. Chatterjee wrote.
Source: Dr. Cynthia Chatterjee written testimony, Oct. 7, 2023
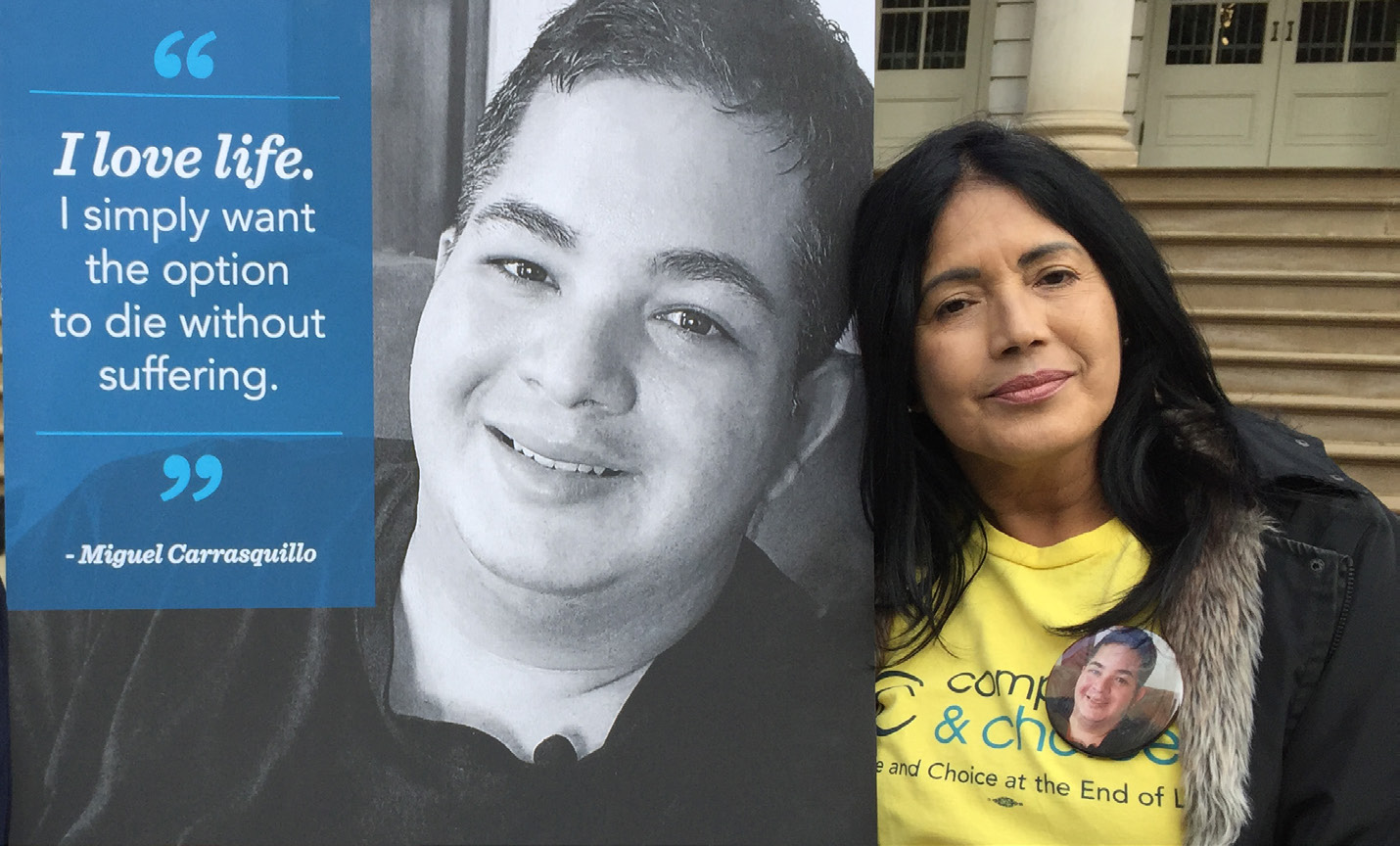
ILLINOIS/NEW YORK/PUERTO RICO STORYTELLER
Nilsa Centeno
Nilsa Centeno’s only son, Miguel Carrasquillo, a former chef in Chicago and New York, died at age 35 from an aggressive form of brain cancer on June 5, 2016. Although he went home to die in his native Puerto Rico, where medical aid in dying has not been authorized, he advocated his wish for access to this end-of-life care option until his last breath.
“During the last months of his life, Miguel spoke to me about his desire to ingest medication to peacefully end his suffering so he could take his last breath holding my hand at home … I must confess that when Miguel first let me know he was considering medical aid in dying, I involuntarily shook my head saying no. But as I watched my son suffer, I realized that our Lord had no desire for my child, His child, to suffer needlessly,” Centeno wrote in a Chicago Tribune op-ed.
Source: Chicago Tribune op-ed: “Terminal cancer made my son suffer. I urge state lawmakers to pass death with dignity legislation,” Jun. 11, 2021

MASSACHUSETTS PALLIATIVE CARE PHYSICIAN
Dr. Jeff Zesiger
When Massachusetts palliative care physician Dr. Jeffrey Zesiger began his career, he felt so confident in hospice and palliative care that he believed the option for medical aid in dying was unnecessary. However, the more familiar he became with end-of-life care, the more he felt his confidence wavering.
“Living is complicated, and so too is dying. I noticed some patients were not as comfortable as they wished, but I felt it was the best we could do given a tough situation. Over the years, it became harder to rationalize these less than ‘good deaths.’ Excellent palliative care and hospice teams are not perfect, nor are they available everywhere. My concern grew when some people used violent means to end their intolerable suffering … We have a duty to comfort, listen and seek solutions for suffering. [Medical aid in dying] is just one tool I need in my doctor’s bag.”
Source: The Worcester Telegram op-ed: “Zesiger: Make med aid in dying available in Mass.,” Mar. 5, 2023

NEVADA STATE SENATOR
Edgar Flores
As a new assemblymember, Senator Flores was unsure of the bill and did not originally support medical aid-in-dying legislation when it was introduced in Nevada. After learning more about the issue and hearing testimonies of terminally ill Nevadans, he became a supporter and the lead bill sponsor.
“Working with Compassion & Choices helped me understand the importance of expanding options at the end of life. The first-hand knowledge and experience of working with individuals, families and the community on these important issues, empowered me to use my leadership in the Nevada Senate to help ensure people are aware about getting the care they want – or do not want, so they can chart their end-of-life journey.”
Source: Personal remarks approved by Sen. Flores, Nov. 15, 2023

NEW YORK UNIVERSITY LANGONE BIOETHICIST PROFESSOR
Dr. Arthur Caplan
Bioethicist Dr. Arthur Caplan, NYU Langone professor and founder of the Division of Medical Ethics Department of Population Health at NYU Grossman School of Medicine, initially worried about the ethical implications of medical aid in dying. But after watching how medical aid-in-dying laws were successfully implemented, with no documented cases of abuse or coercion, it solidified his belief that medical aid in dying is an ethical, compassionate end-of-life care option.
“I initially opposed [medical aid in] dying but I changed my mind. We have had 20 years of this now, starting with Oregon and then Washington [state], and the checks and balances in these laws work well. If it can work in California without abuses for three or four years, you’ll see expansion to more states,” said Dr. Caplan.
Source: Religion News Service, “6 Life and Death Questions for Ethicist Arthur Caplan“, Jun. 30, 2016
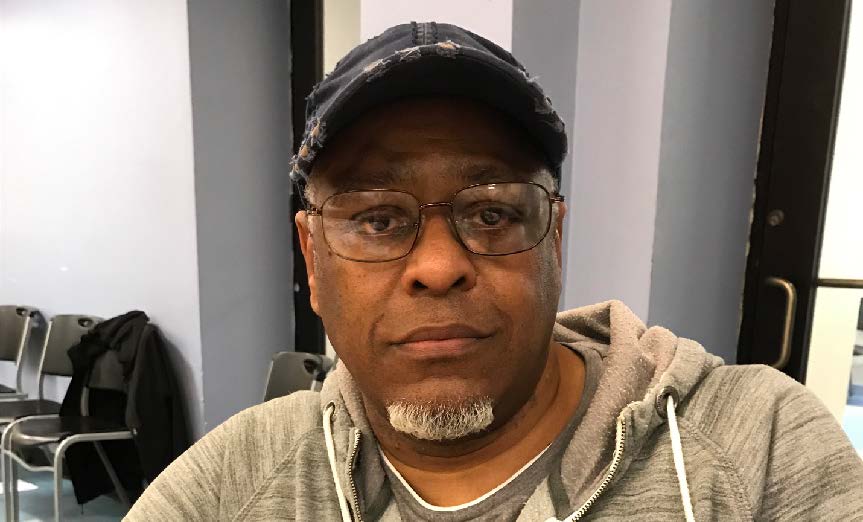
NEW YORK STORYTELLER
Anthony Randolph
Anthony Randolph was initially opposed to medical aid in dying, but after watching his brother suffer in prolonged agony from lung cancer, he became a convert.
“I understand why people oppose medical aid in dying. I was one of them. But I ask you to spend 24 hours with someone who is dying and suffering. There’s no way you’re going to see all that and not support the option of medical aid in dying. God gives us the option of making the decision for ourselves for a reason. Every terminally ill person deserves to have the option — the decision is between you and your God. My brother suffered needlessly, and the whole family, including James’ children, watched. We suffered by watching. I still think about it. I still think about watching him take his last breaths. There has to be a better way. That’s why I support New York’s Medical Aid in Dying Act.”
Source: Anthony Randolph’s story, Apr. 2019

OREGON HOSPICE ASSOCIATION FORMER CEO
Ann Jackson
Ann Jackson, former CEO and chief spokesperson of the Oregon Hospice Association, was opposed to Oregon’s 1994 Death With Dignity Act ballot initiative, the first medical aid-in-dying law in the nation, and voted yes on a 1997 ballot initiative to repeal it that failed to pass.
“I had voted against the law twice, but by 1998, when it was implemented, I had spent the last several years making sure that every Oregonian would have access to hospice and palliative care AND the Oregon Death with Dignity Act. I had voted against the referendum because I believed it was unnecessary if terminally ill Oregonians had access to high-quality hospice and palliative care — and received it
Source: Quote via email Nov. 22, 2023

WASHINGTON D.C. COUNCIL MEMBER
Kenyan R. McDuffie
Prior to the passage of the Washington, D.C. Death with Dignity Act, D.C. Council Member Kenyan R. McDuffie grappled with his own feelings about medical aid in dying in a Nov. 1, 2016 council meeting covered by The Washington Post. His experience witnessing the death of his father earlier that year made the difference for McDuffie.
“My family had to watch him suffer, and I wouldn’t wish that on anyone else. But I’m not making this vote today based on my own story because there are thousands of other people throughout the district who have had the same experience, and they should be able to make and decide for themselves what they want to happen when their loved one is terminally ill.”
Source: The Washington Post, “D.C. Council gives initial approval to a bill to let terminally ill patients end their lives,” Nov. 1, 2016

WASHINGTON, D.C. REVEREND
Charles McNeil
Reverend Charles McNeil of Unity Baptist Church in Washington, D.C. heard many rumors in the African American community when the 2016 District of Columbia Death With Dignity Act was introduced, and was initially skeptical about the benefits of such a bill. He decided to educate himself on the facts of the proposed bill.
“And once I got the full knowledge of what the bill really was and began to understand and began to read stuff for myself, then I became a convert. I said, this is something that is needed in the African American community. It’s not necessarily focusing on dying, but it’s focused on preparing to die, and it’s something that is lacking in the African American community, especially in our churches … But we have to be able to have an honest and open conversation.”
Source: YouTube: “My Faith Journey on the Subject of Medical Aid in Dying,” [1:21-1:57], Apr. 5, 2023

WASHINGTON D.C. FORMER COUNCIL MEMBER
Brandon T. Todd
When former Washington, D.C. Council member Brandon T. Todd met vocal medical aid-in-dying advocate Mary Klein after knocking on her door while canvassing for reelection, he told her he was firmly against the then-proposed Washington, D.C. Death With Dignity Act for religious reasons; he believed it was only God’s duty to give or take life. However, when Klein asked Todd to have a conversation with her on the topic of medical aid in dying, they spoke for an hour, and his stance on this end-of-life care option became supportive.
“It wasn’t easy for me to come to the decision … But her story just — it stuck out. I thought to myself, well, somebody in my family could be in this position. I don’t know what I would do … But I think having the option, I think it’s okay. I think it’s okay.”
Source: The Washington Post, “She fought cancer and Congress for D.C.’s right-todie law. Would she be able to use it?” Dec. 25, 2018


