What does the data show?
Beginning in August 2020, federal guidance required that all labs testing for the coronavirus collect and report on people’s race and ethnicity. Until then, such data was limited. Even today, data on race/ethnicity is available for roughly 63% of COVID-19 cases and 83% of COVID-19 deaths and states continue to report this data inconsistently.1
National Data
As of July 16, 2021, American Indians and Alaska Natives, African Americans and Latino Americans are about three times more likely to require hospitalization after COVID-19 infection and twice as likely to die from the coronavirus than are white Americans.2
Local/State Data
The local/state data is also important. Each of the examples below shows the disproportionate ratio of deaths to the share of the total population for the state among different racially and ethnically diverse populations: 3
- In Michigan, African Americans comprise 14% of the population, but make up 23% of overall COVID-19 deaths for the state.
- In California, Latinos make up 63% of all COVID cases and 48% of deaths, but make up 40% of the state population.
- American Indians and Alaska Natives die at disproportionate rates in more than a dozen states. For example, in New Mexico, they comprise 9% of the population but account for 31% of COVID-19 deaths for the state. The figures are similar in Montana, where American Indians and Alaska Natives comprise 6% of the population but account for 17% of deaths.
- Among Asian Americans, data show disproporate death rates in Nevada, Utah and Alaska, where they comprise 6% of the state’s population but account for 10% of the deaths.
Risk for COVID-19 Infection, Hospitalization and Death by Race/Ethnicity Reported Through July 16, 2021
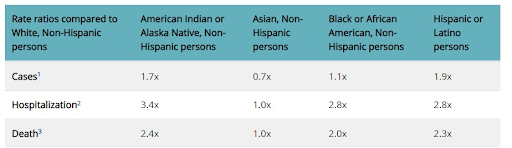
Source: Centers for Disease Control and Prevention, COVID Data Tracker as of July 16, 2021.
Why do these disparities exist?
The underlying causes of health disparities experienced by racially and ethnically diverse populations are complex. Factors that play a role include racism, bias and discrimination, economic and educational disadvantages, healthcare access and quality, individual behavior and overall health. In the context of Covid-19, certain communities face increased risk for experiencing serious illness due to the coronavirus. Some of the factors that increase risk fall into three primary categories: 1) economic and social circumstances; 2) access to testing and treatment; and 3) underlying health conditions. 4
- Economic and Social Circumstances
Where people live, work, attend school, play and pray have a strong influence on health outcomes. In some communities, the following factors may play a role in the COVID-19 disparities:
- Lower median incomes which lessens the chance of having a financial cushion to absorb income declines; thus, reducing the likelihood of health coverage and income for healthcare.5
- Employed in front-line service industries deemed essential, such as grocery store workers and delivery drivers, resulting in greater exposure to the coronavirus.6
- Limited paid sick leave, leaving people more likely to continue to work even when they do get sick for any reason.7
- Living in densely populated areas, making it more difficult to practice social distancing.
- Disproportionate representation in jails, prisons, and detention centers, which have specific risks due to congregate living, shared food service and more.8
- Historic trauma, such as the continued fall out of state and local laws that enforced racial segregation and discrimination among Blacks in the United States or the ongoing impact of colonization on American Indians.
- Access to Testing, Treatment and Vaccines History shows that diverse patients receive less care and often worse care than white patients.9 The reasons are complex:
- Language and cultural barriers reduce the likelihood people will seek out healthcare providers and fully understand and adhere to treatment regimens.
- Not having health insurance which lessens the chance of receiving adequate healthcare.10
- Long-standing distrust of the health care system, stemming from incidents such as the U.S. Tuskegee syphilis study which provided sham treatments to African American men and thus leading to avoidance of healthcare.
- Implicit bias or explicit discrimination by healthcare systems and providers, ultimately impacting who gets testing and treatment first.11
|
- Underlying Health Conditions
Many racial and ethnically diverse populations often
- Report fair to poor health, putting them at greater risk for the coronavirus.
- Have higher rates of certain health conditions that put them at higher risk for experiencing serious illness if they contract COVID-19, including asthma, diabetes, HIV/AIDS, heart disease and obesity.12
How can I protect myself, my family and my community?
There are things you can do now to protect yourself and your family: reduce your risk, get care safely, and plan your care, including end-of-life care.
Know Your Risk
Know whether you are at higher risk. In general, people with the following conditions may be at higher risk:
- Older adults
- People who live in a nursing home or long-term care facility
- People with chronic lung disease, such as asthma or COPD, heart disease, kidney disease or liver disease, or diabetes
- People with a weakened immune system by cancer, smoking, bone marrow or organ transplantation, HIV/AIDS
- People with severe obesity
Reduce Your Risk
Know how to protect yourself and others:
- Consider getting a COVID-19 vaccine, which can help to prevent you from getting the coronavirus and to reduce the severity if you do contract the virus.
- Follow CDC’s guidelines on how to protect yourself .
- Stay home as much as possible.
- Try to keep space between yourself and others. On public transportation, look for a spot away from people if possible.
- Avoid crowds.
- Avoid touching your face, and use a mask that covers your nose and mouth when you are in public places.
- Wash your hands often; use alcohol-based gel when soap and water are not available.
Get Care Safely
If you experience a health problem and need care, here are some suggestions.
- If you have health coverage, contact your health provider to learn how to seek healthcare safely. Ask whether you can use telehealth to reduce your risk, and, learn more about key issues and steps to prepare for a telehealth visit.
- If you don’t have health coverage, contact your local health clinic. Use the following:
- Find a Health Center to locate a community health center in your area. Ask if they offer telehealth appointments.
- Digital Health Directory to find telehealth (referred to as telemedicine in the directory) options near you.
- Learn about the different COVID-19 treatment options , such as ventilators, respiratory care, and other non-invasive treatments in the event you contract the virus.
Plan Your End-of-Life Wishes
Discuss and document your end-of-life preferences with loved ones. Consider end-of-life planning options as well as hospice and palliative care. Now is the time to have those hard conversations with family members about your wishes. Use Compassion & Choices tools to get started (available in English and Spanish):
- COVID-19: Advance Care Planning – step-by-step instructions for planning and documenting decisions about your end-of-life care.
- Plan Your Care Resource Center – toolkits, factsheets, links to state-specific advance directives forms and more to get you started.
What can our society do to reduce disparities in end-of-life care?
Collecting accurate nationwide data by race and ethnicity will be important to understanding how COVID-19 is affecting communities and to informing end-of-life care response efforts. Due to concerns with reporting methodology, the COVID Tracking Project has teamed up with American University to establish the COVID Racial Data Tracker to record and analyze racial data on the pandemic within the United States.
Beyond data collection, Compassion & Choices offers the following policy and programmatic recommendations specific to improving end-of-life care and choices:
- Address bias and discrimination within healthcare systems related to patient–provider interactions, treatment decisions, treatment adherence and patient health outcomes.
- Support the development of on-demand, low cost or no cost digital tools that help people access health information and end-of-life treatment and care.
- Create culturally competent communication messages tailored to specific populations through methods that increase usage.
- Increase access to telehealth and virtual care services that are on-demand and community-based.
- Expand community-based testing centers and providers, employ mobile testing sites in underserved communities and prioritize access to those at increased risk of exposure.
Prioritize and support research that identifies the practices, policies and conditions that account for disparate differences in disease progression, end-of-life care and recovery for COVID-19. Consider participating in a free COVID-19 symptom tracker research program, such as the Duke Community Health Watch.
Learn More
From Compassion & Choices:
- COVID-19: Understanding Your Options / Español
- COVID-19: Using Telehealth to Reduce Your Risk / Español
- COVID-19: Advance Care Planning / Español
- COVID-19: Addendum to Your Advance Directive / Español
COVID-19: Dying in the Age of the Pandemic / Español
From Other Organizations:
COVID-19 Rates
- CDC, Weekly Updates by Select Demographic and Geographic Characteristics
- Coronavirus Case Rates and Death Rates for Latinos in the United States
- Coronavirus (COVID-19) (Indian Health Service)
- COVID-19 Has Infected and Killed Black People At Alarming Rates. This Data Proves It.
- The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.
Resources
- COVID-19 Crisis Highlights Ways to Combat Health Disparities for People of Color
- Asian Americans Advancing Justice. Coronavirus/COVID-19 Resources To Stand Against Racism
- Coronavirus Disease 2019 (COVID-19) (English and Spanish), National Alliance for Hispanic Health
- Ten Equity Implications of the Coronavirus COVID-19 Outbreak in the US , NAACP
- Federal Response to Indian Country: COVID-19, Indian Health Service
- COVID-19 and Equity, American Public Health Association
- COVID-19: Update and Impact on African American and Vulnerable Populations (webinar), Society for Public Health Education
- Resource Guide to COVID-19, Society for Public Health Education
From the Centers for Disease Control and Prevention (CDC):
- COVID-19 Vaccines / Español
- How COVID_19 Spreads / Español
- How to Protect Yourself and Others / Español
- What to Do If You Are Sick / Español
- Symptoms of COVID-19 / Español
References
- Centers for Disease Control and Prevention. COVID Data Tracker, Demographics, as of July 16, 2021. Available at: https://covid.cdc.gov/covid-data-tracker/#demographics .
- Centers for Disease Control and Prevention, COVID Data Tracker as of July 16, 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- Kaiser Family Foundation. COVID-19: Cases and Deaths by Race/Ethnicity, as of July 14, 2021. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/state-covid-19-data-and-policy-actions/#raceethnicity
- Artiga S, Garfield R, Orgera K. Communities of Color at Higher Risk for Health and Economic Challenges due to COVID-19. Kaiser Family Foundation 2020, Apr 7. Available at: https://www.kff.org/disparities-policy/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/
- U.S. Census Bureau. Real Median Household Income by Race and Hispanic Origin. 1967-2017. Available at: https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf .
- US Bureau of Labor Statistics, Report 1082, Labor force characteristics by race and ethnicity, 2018, October 2019, https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htm .
- US Bureau of Labor Statistics, Report 1082, Labor force characteristics by race and ethnicity, 2018. October 2019. https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htm .
- CDC, COVID-19 in Racial and Ethnic Minority Groups. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html .
- Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press; 2003. Available at: https://www.ncbi.nlm.nih.gov/pubmed/25032386.
- Bartel AP, Kim S, Nam J, Rossin-Slater M, Ruhm C, Waldfogel J. Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets, Monthly Labor Review, U.S. Bureau of Labor Statistics, January 2019. https://doi.org/10.21916/mlr.2019.2.
- Ziad Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 25 Oct 2019;Vol. 366, Issue 6464, pp. 447-453. Available at https://science.sciencemag.org/content/366/6464/447.
- Samantha Artiga and Kendal Orgera, Key Facts on Health and Health Care by Race and Ethnicity, (Washington, DC, KFF, November 2019), https://www.kff.org/report-section/key-facts-on-health-and-health-care-by-race-and-ethnicity-health-status/


